Relevant Board Review Material from Publications Updates 1 - 50

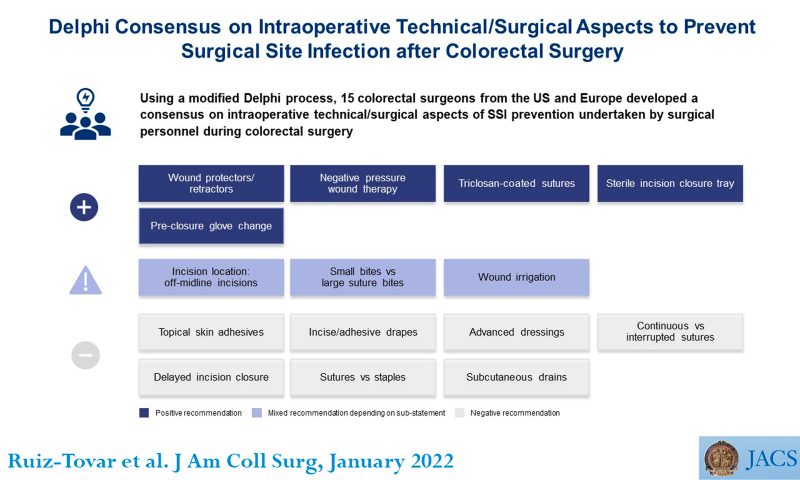
Surgical Site Infections (Publications Update # 7)

Pelvic Exenteration (Publications Update # 7)
- Complication rates are high after exenteration
- MSKCC Paper (Pubmed)
- 20/100 patients developed a pelvic abscess
- 23/100 urosepsis
- 14/100 hydronephrosis
- 6/100 disruption of urinary conduit
- 10/100 VTE events
- 40/100 wound infection
- Leiden (Netherlands)(Pubmed
- 19/90 sepsis
- 1/90 died
- 11/90 wound infection
- 15/90 urinary conduit leakage
- 6/90 VTE
- 4/90 bowel leaks
- 12/90
- 19/90 sepsis
- MSKCC Paper (Pubmed)
2-year and 5-year PFS 41% and 32% in the Leiden series patients undergoing exenteration for curative intent.
IVC Filters (Publications Update # 8)
If a patient needs surgical intervention after a recent VTE, the placement of IVC filters is recommended. These IVC filters can be permanent or retrievable.
Most of the IVC filters placed nowadays are retrievable IVC filters. However, the retrieval rate of these filters is low (~10% in some publications). Structured programs to follow up on these patients increase the rates of retrieval. Here is what you need to know as a gyn oncologist about the VTE filters:
- An IVC filter should be considered for patients with acute PE or acute DVT who have contraindications to anticoagulation. This contraindication could be temporary, i.e., necessary surgery (if surgery cannot be postponed)
- When the risk of PE is mitigated, retrieve the filter.
- The FDA recommends retrieval of the filter within 29-54 days after placement if the risk of acute PE has passed - based on this study.
Full Summary

Low-Grade Ovarian Cancer (Publications Update # 9)


Two articles focus on the effectiveness of chemotherapy in low-grade ovarian cancer. Both articles show that Bevacizumab has a response rate of nearly 30-40% in this patient population. The MITO 22 trial notes that perhaps adding Bevacizumab to carboplatin and taxol prolonged the PFS both in upfront and first recurrence.
Manning-Geist et al.'s article notes that the response rate in patients receiving carboplatin and taxol as NACT, the response rate is 9%. This is not infrequent when chemotherapy is started based on ascites fluid showing PAX-8 positive cells. A tissue biopsy can avoid this situation.
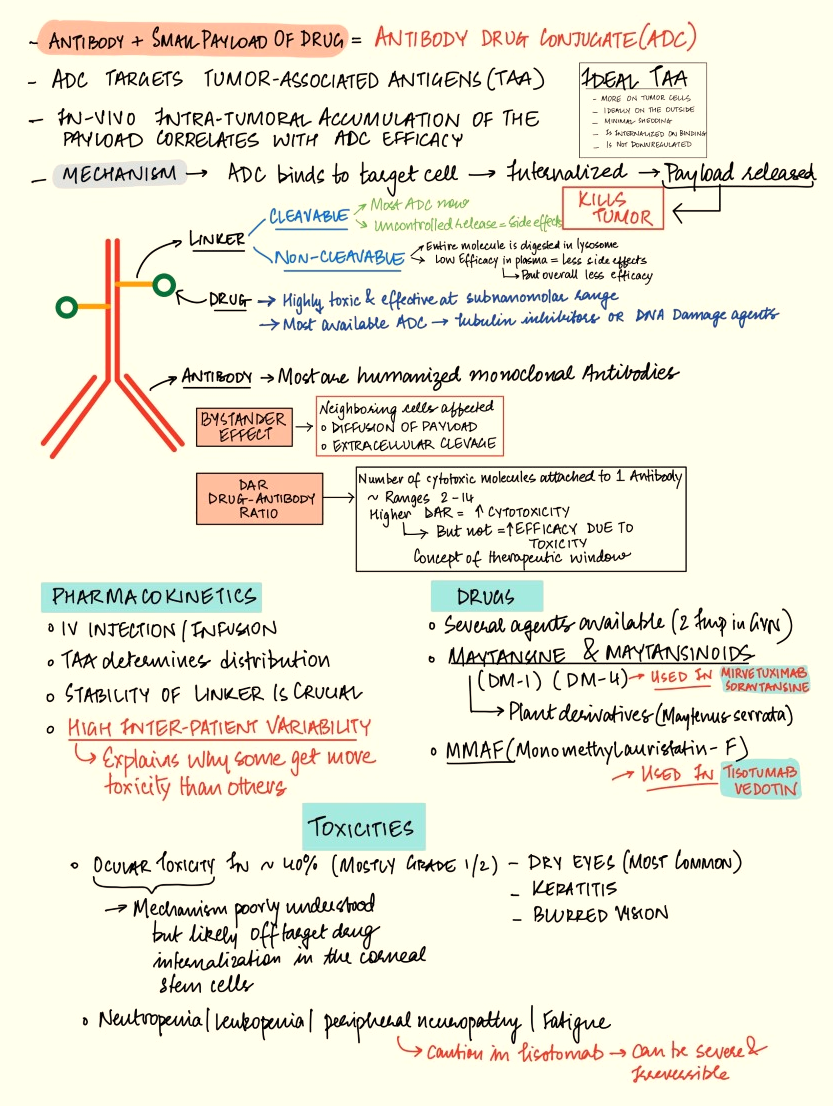
ADC Cheatsheet (Publications Update # 10)
Ovarian Transposition (Publications Update # 11)
After about 20-30 Gy, the rate of ovarian failure is 97%. In cervical cancer literature, a recent systematic review analyzed 28 studies and reported that after curative intent radiation, ovarian preservation rates were around 50% (range 41-60%).
The procedure involves transection of the utero-ovarian ligament and dissection of the peritoneum between the IP and the ureter to mobilize the ovary and IP ligament. Often, ovaries are attached to the anterior abdominal wall in the para-colic gutter using sutures or hernia-tacks (caution they can cause more pain - anecdotal experience). Higher and farther may or may not be the best approach (limited data) - more tension on the pedicle = higher probability of failure. So outside the pelvic brim seems to be a reasonable place in the era of IMRT.
This new study (as a systematic review) looks at the efficacy of ovarian transposition in a completely different (~60%). Complications are relatively low. This study did not include the risk of metastasis to the ovaries, but the risk of ovarian involvement can be as high as 10% in sigmoid colon malignancies.

Antiemetics (Publications Update # 13)
The ASCO guidelines are a great resource: ASCO GUIDELINES
Highly Emetogenic
| Medication | Dosage | Administration |
|---|---|---|
| NK1 | Aprepitant 125 mg oral | On day 1 |
| Aprepitant 80 mg oral | On days 2-3 | |
| Fosaprepitant 150 mg IV | On the day of infusion | |
| See others in ASCO guidelines | ||
| 5-HT3 | Ondansetron 8 mg | On the day of chemotherapy |
| PRN | After that | |
| Dexamethasone | 12 mg | On the day of infusion |
| 8 mg oral | Daily on days 2-4 | |
| Olanzapine | 10mg or 5 mg oral | At bedtime |
Carboplatin at AUC >4
Carboplatin at AUC > 4 has a special designation as a moderately high emetogenic drug where NK1 inhibitor use is ok (in addition to 5 HT3 + Dex), but olanzapine is optional.
Moderately Emetogenic
| Medication | Dosage | Administration |
|---|---|---|
| 5-HT3 | Ondansetron 8 mg | On the day of chemotherapy, 2 doses |
| PRN | After that | |
| Dexamethasone | 8 mg | On the day of infusion (oral or IV) |
| 8 mg oral | Daily on days 2-4 (if agent has known risk of delayed nausea) |
Low Emetogeic
| Medication | Dosage | Administration |
|---|---|---|
| 5-HT3 | Ondansetron 8 mg | On the day of chemotherapy |
| PRN | After that | |
| Dexamethasone | 8 mg | On the day of infusion |
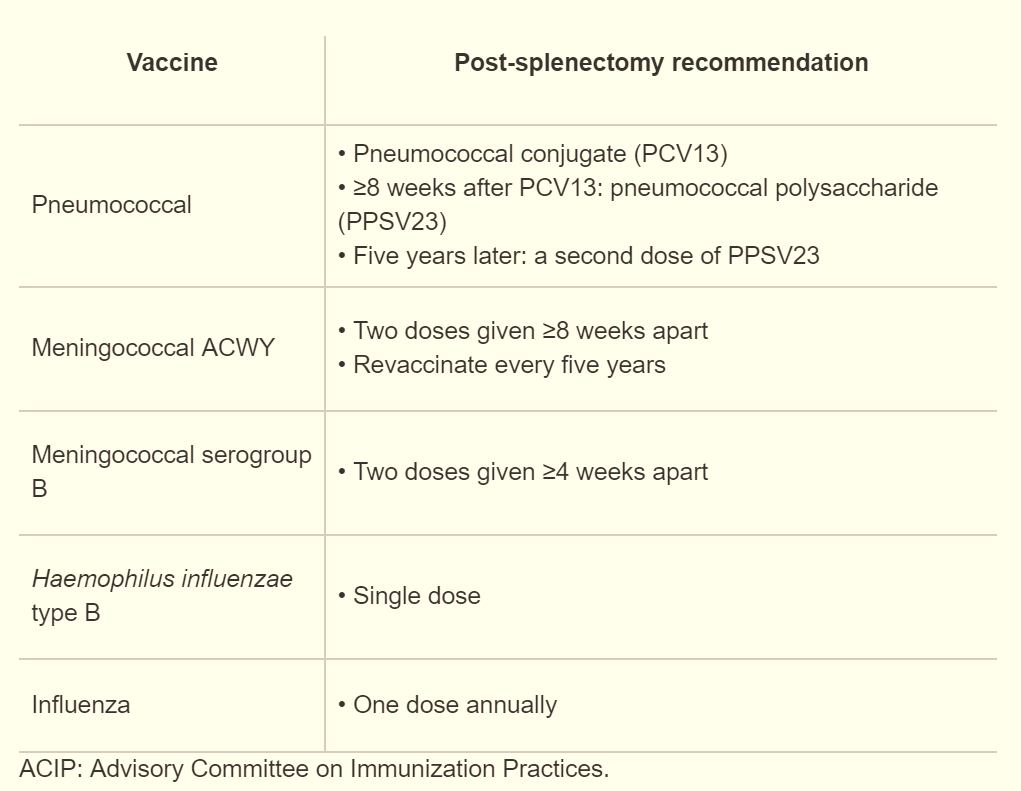
Splenectomy (Publications Update # 15)
You can head to Publications Update # 15 to watch a video on splenectomy.
Don't waste your time with tying the vessels, just use a vascular load of staples using EndoGIA stapler
Vaccinations Guide Post Splenectomy:
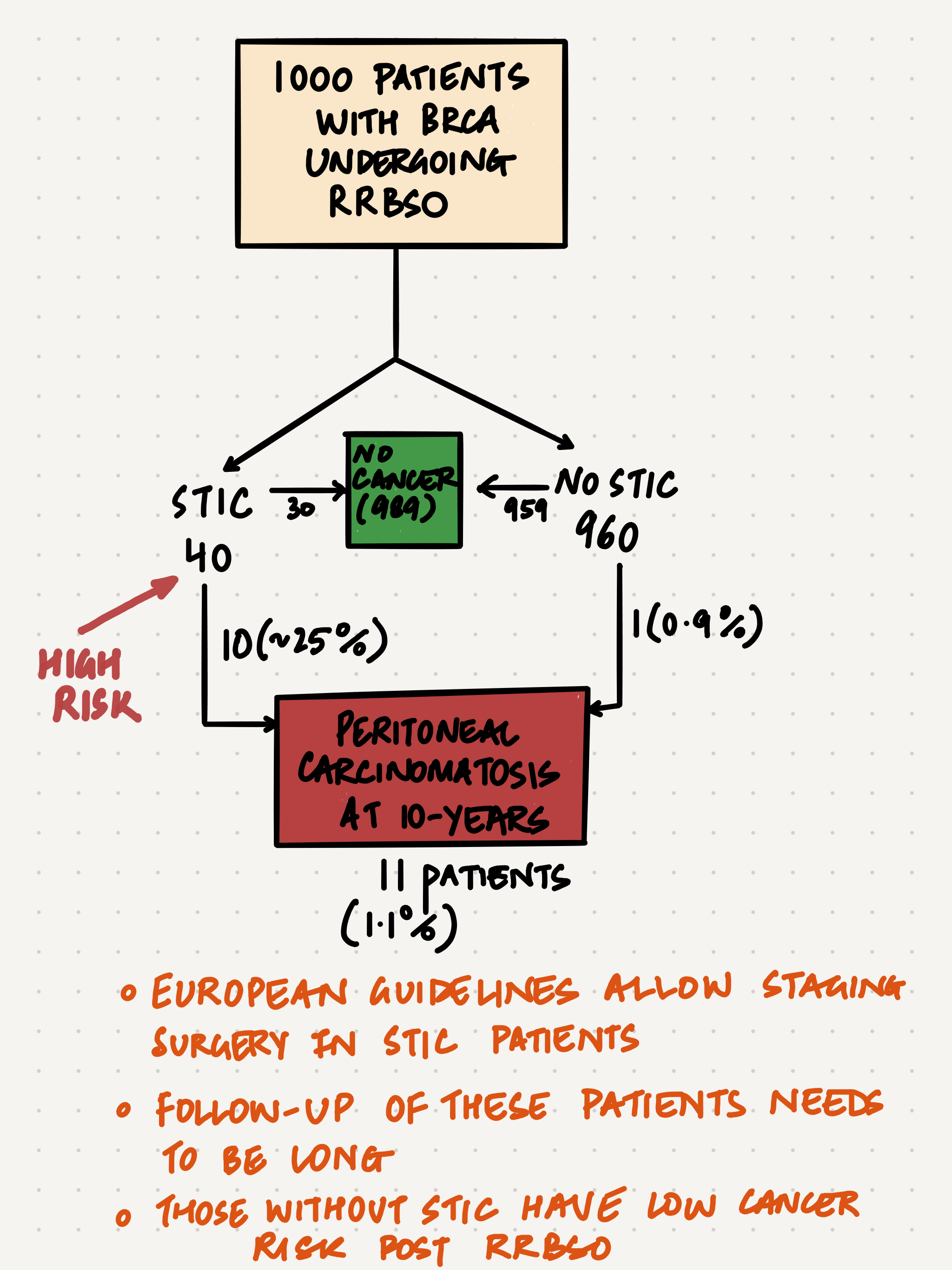
STIC Mini-tutorial (Publications Update # 18)
The risk-reduction salpingo-oophorectomy literature is complicated, but knowing the key numbers can help. Some percentages are rounded to make them easy to remember.
Let's approach this subject with a starting point of 1000 women with BRCA mutation undergoing rrBSO.

Pulmonary Embolism (Publications Update # 22)
Read this clinical review paper published in NEJM last year.

Relevant key points in the management of pulmonary embolism in cancer patients from this paper and the updated CHEST guidelines (available here) include:
- For cancer patients with VTE, use DOACs (e.g., apixaban, edoxaban, or rivaroxaban) during treatment (strong recommendation, moderate-certainty evidence). Exception: luminal gastrointestinal malignancy patients should use apixaban or low-molecular-weight heparin to reduce bleeding risk.
- Rate of recurrent VTE with the use of DOAC 5.2% vs. LMWH 8.2% (RR 0.62, 95% CI 0.43-0.91)
- Major bleeding rate DOAC 4.3% vs. LMWH 3.3%, not statistically significant
- Exception, major GI bleeding rates were higher in patients receiving edoxaban, or rivaroxaban

Admission to the hospital is not warranted given hemodynamic stability and low simplified Pulmonary Embolism Severity Index (PESI) score (read the NEJM paper for more info on this)
Stoma Guidelines (Publications Update # 23)
These guidelines from the American Society of Colorectal Surgeons will answer most of your questions and question most of your practices.
Important Points from the Clinical Practice Guidelines
- Loop Ileostomy vs. Transverse Colostomy: In most cases, Loop ileostomy is preferred over transverse loop colostomy for temporary fecal diversion.
- Use of Antiadhesion Materials: Antiadhesion materials may be used to decrease adhesions at temporary ostomy sites.
- Use of Mesh: Lightweight polypropylene mesh may be placed at the time of permanent ostomy creation to decrease parastomal hernia rates.
- Extraperitoneal Tunneling: Extraperitoneal tunneling of end colostomies may decrease parastomal hernia rates.
Preoperative Marking
Key Points:
- Preoperative stoma site marking is recommended for all patients undergoing planned ostomy surgery.
- When selecting a location for the ostomy barrier, it's important to choose a spot that is at least two inches away from bony areas, the midline, creases, scars, and folds. This will provide enough space for the barrier to stick properly. Let the ostomy barrier serve as a guide when choosing the right spot.
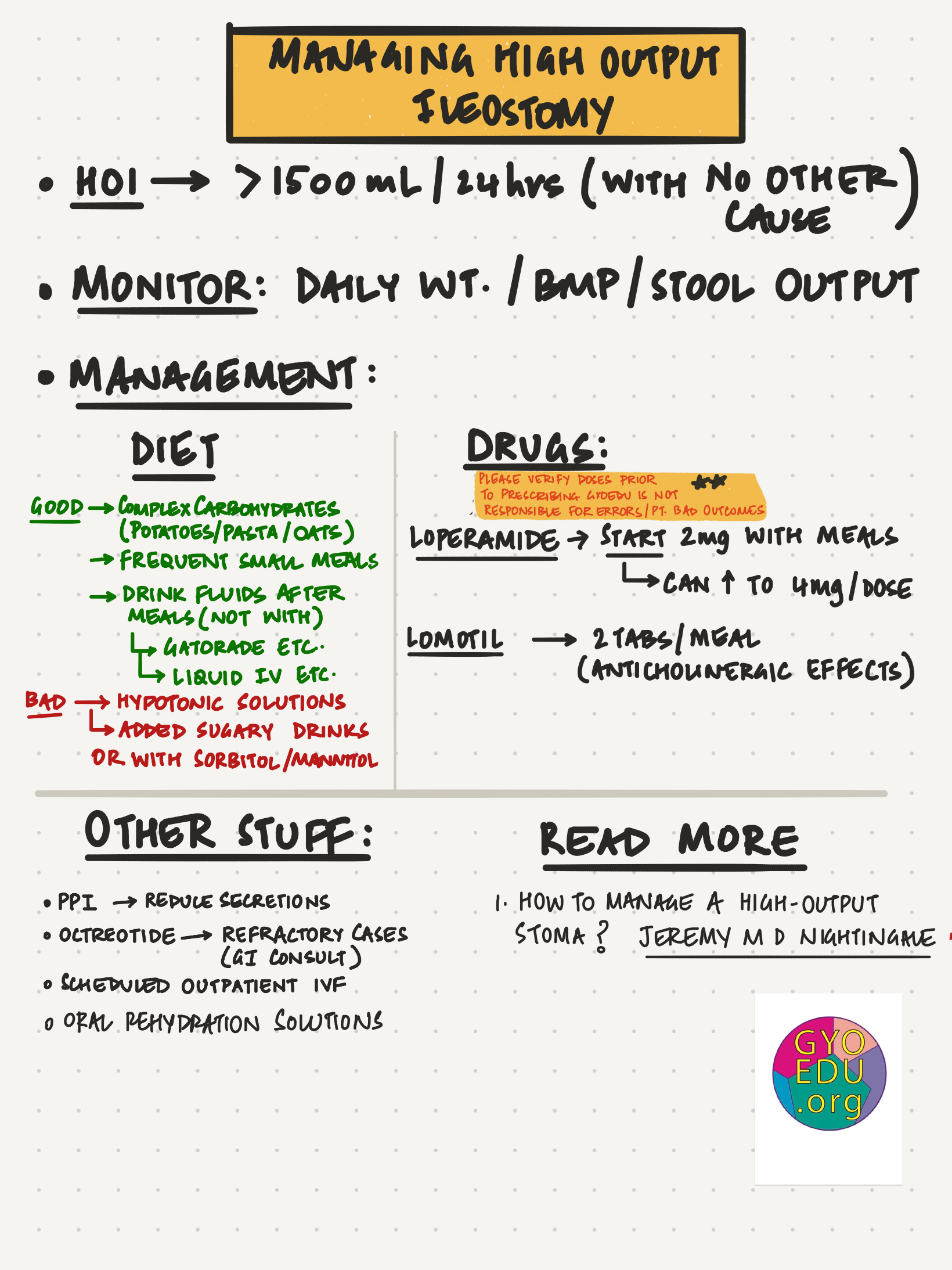
High Output Ileostomy (Publications Update # 23 )
Key Points:
- Ensure good skin protection/bag fitting.
- Exclude causes other than a short bowel (e.g., obstruction).
- Rehydrate and stop thirst.
- Restrict oral hypotonic fluid.
- Sip a glucose/salt solution +/- magnesium supplements.
- Start loperamide (high dose) before food.
- Start a proton pump inhibitor (especially if a net ‘secretory output’).
- Consider reducing oral insoluble fiber intake.
- Monitor random urinary sodium concentration and serum magnesium.
- Patients with a short bowel (less than 2 m remaining) needing parenteral support may be considered for a glucagon-like peptide-2 analog.
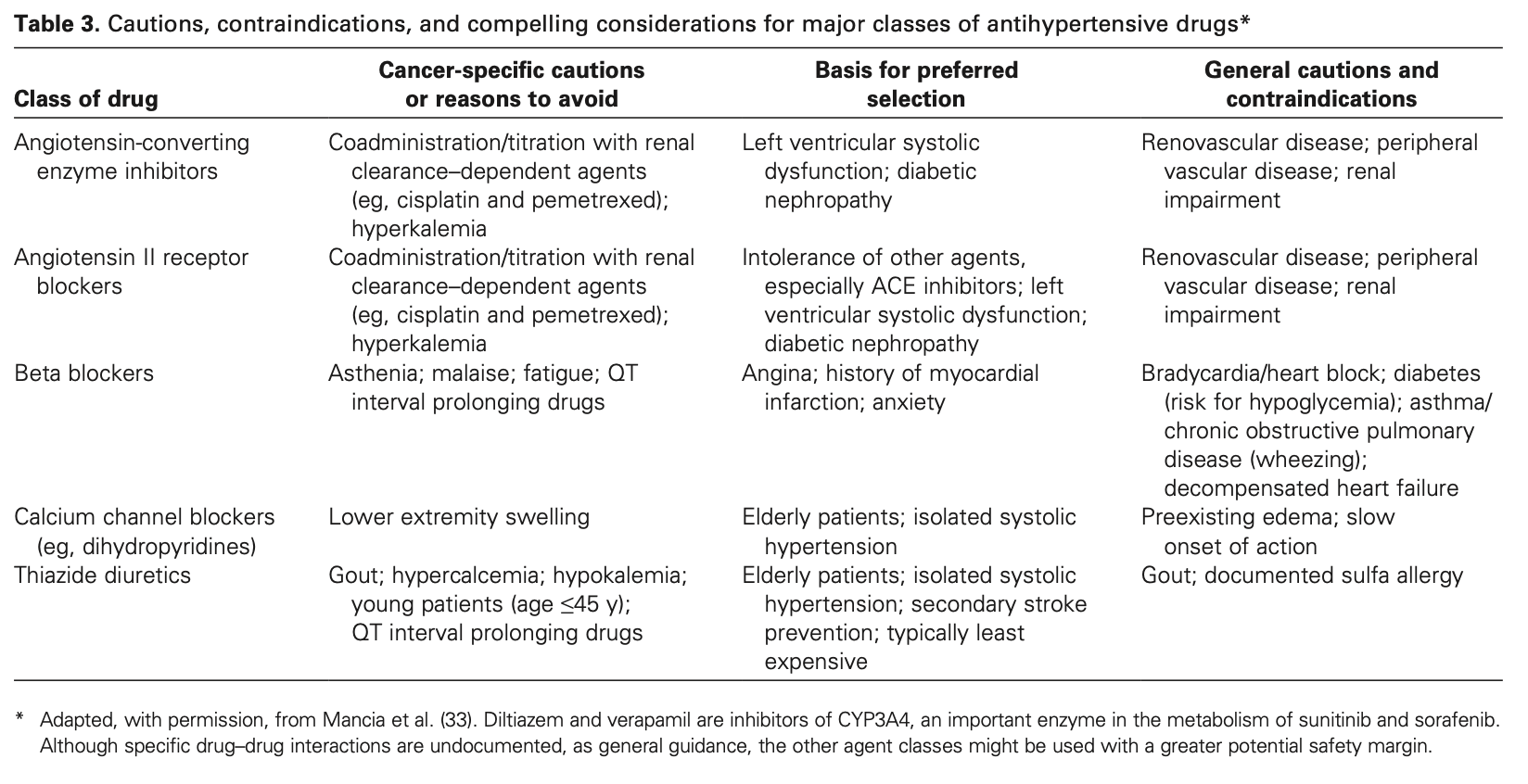
Antihypertensive in Oncology (Publications Update # 33)
Trauma Survival Guide (Publications Update # 35)
Chemotherapy Reactions (Publications Update # 37)

This is an excellent summary of chemotherapy reactions. by the SGO Clinical Practice Statements group. However, I wish that they included two additional elements in this summary
- 3 hours infusion of Carboplatin to prevent hypersensitivity reactions: Watch this lecture to learn more about why and other details of managing delayed hypersensitivity reactions by platinum
- Prevention of Taxol-related reactions: Some older data suggest that oral dexamethasone (started 24 hours before infusion) is more effective than a single IV dose given during infusion. A meta-analysis of 6 studies that included 1347 patients noted that the oral regimen of dexamethasone started 24 hours before infusion lowered the odds of developing severe hypersensitivity reactions by half.

TPN (Publications Update # 39)
Guidelines

Summary Points:
- Nutrition Status Assessment :
- Malnutrition can be diagnosed by considering the patient's nutrition history, performing periodic nutrition assessments, and conducting a physical examination during fistula diagnosis. Serum protein concentrations may provide prognostic outcome indicators.
- Preferred Route of Nutrition Therapy:
- After stabilization of fluid and electrolyte balance, oral diet or enteral nutrition (EN) may be feasible and tolerated in patients with low-output ECF (<500 mL/d).
- Patients with high-output ECF (>500 mL/d) may require Parenteral Nutrition (PN) to meet fluid, electrolyte, and nutrient requirements to support spontaneous or surgical closure of the ECF.
- Protein and Energy Intake Recommendations:
- Protein provision is suggested at 1.5–2.0 g/kg/d, and energy intake should be based on the patient’s energy requirements from the nutrition assessment.
- More protein (up to 2.5 g/kg/d) may be required in patients with the fistula and high fistula output.
- Use of Somatostatin or Somatostatin Analogue:
- Somatostatin analog is recommended in adult patients with high-output (>500 mL/d) ECF to reduce effluent drainage and enhance spontaneous closure.
- Indication for Home Parenteral Nutrition (HPN):
- HPN is suggested for medically stable patients with manageable fistula output and high-output ECF (>500 mL/d) when surgical repair is not yet advised.
Road to Carboplatin and Taxol (Publications Update # 44)
For board exams, you don't need to know much more than the basics of these trials. I would spend more time on GOG 218, GOG 252, and dose-dense therapy trials if they arise during the discussion.
| Name of Trial | Year Published | Control Arm with Outcomes | Experimental Arm(s) with Outcomes | P-Values or HR | Conclusion |
|---|---|---|---|---|---|
| GOG 111 | 1996 | Cisplatin & Cyclophosphamide: OS 24 months | Cisplatin & Paclitaxel: OS 38 months | 36% reduction in mortality | Paclitaxel with Cisplatin significantly improved PFS and OS. |
| SCOTROC | 1999 | Paclitaxel & Cisplatin: PFS 15.4 months | Docetaxel & Cisplatin: PFS 15.1 months | Efficacy similar less neuropathy but more myelosuppression with Docetaxel | Docetaxel is a reasonable substitute for Paclitaxel especially in patients at risk of neuropathy. |
| GOG 132 | 2000 | Cisplatin alone: PFS 16 months, OS 30 months | Paclitaxel alone: PFS 11 months, OS 26 months; Cisplatin & Paclitaxel: PFS 14 months, OS 26 months | Taxol worse alone - significant; No difference between cis and cis/taxol; Worse toxicity with cis alone at 100mg/m2 | |
| ICON3 | 2002 | Carboplatin alone : Median survival 35.4 months | Carboplatin & Paclitaxel: Median survival 36.1 months | PFS and OS similar between groups | Single-agent Carboplatin suggested as preferred therapy due to lower toxicity. |
| GOG 158 | 2003 | Cisplatin & Paclitaxel: PFS 19.4 months OS 48.7 months | Carboplatin & Paclitaxel: PFS 20.7 months OS 57.4 months | PFS: HR 0.88 OS: HR 0.84 | Carboplatin & Paclitaxel reduced progression and death rates with lower toxicity. |
| GOG 114 | 2001 | IV Cisplatin & Paclitaxel: PFS 22.5 months OS 47.6 months | Carboplatin (AUC=9) & IP Cisplatin: PFS 27.6 months OS 59.9 months | PFS: p=0.02 OS: p=0.056 | Dose-intense arm showed improvement in PFS but not in OS. |
| GOG 172 | 2006 | IV Cisplatin & Paclitaxel: PFS 18.3 months OS 49.7 months | IP Cisplatin & IP Paclitaxel: PFS 23.8 months OS 65.6 months | PFS: p=0.05 OS: p=0.03 | IP therapy improved median PFS and OS compared to IV therapy. |
| GOG 218 | 2011 | Carboplatin & Paclitaxel: PFS 10.3 months OS 41.1 months | Bevacizumab with Chemotherapy: PFS 14.1 months OS 43.4 months | PFS: HR 0.717 p<0.001 | Bevacizumab improved PFS but not OS. More toxicity was noted with Bevacizumab. |
| ICON7 | 2011 | Carboplatin & Taxol: PFS 22.4 mos OS 44.6 mos | Carboplatin & Taxol + Bevacizumab: PFS 24.1 mos OS 45.5 mos | Bevacizumab added to primary chemotherapy shows modest PFS benefit and no OS benefit. | |
| GOG 252 | 2019 | IV Carboplatin & Paclitaxel: PFS 24.9 months OS 75.5 months | IP Carboplatin & Paclitaxel or IP Cisplatin: PFS 27.4/26.2 months OS 78. | IP chemotherapy did not improve survival |
*Not shown GOG 262
Mini Tutorial - Adenoma Malignum (Publications Update # 45)
What is Adenoma Malignum?
Adenoma malignum, also known as minimum deviation adenocarcinoma, refers to a highly differentiated form of adenocarcinoma of the cervix. First described in 1870 by Gusserow, it is characterized by its deceptively benign histological appearance, making it difficult to recognize as malignant using the usual criteria for adenocarcinoma of the cervix. A notable characteristic of adenoma malignum is its resistance to radiotherapy.
How is the diagnosis made?
Diagnosing adenoma malignum (minimum deviation adenocarcinoma) involves several steps due to its challenging nature. Clinically, patients often present with symptoms like watery or mucous discharge or abnormal uterine bleeding. Upon physical examination, the cervix is typically firm and indurated. Ultrasonic examination can reveal a multiloculated tumor in about two-thirds of cases.
However, standard diagnostic methods like Pap smears are often inadequate, as they show precancerous or malignant cells in only one-third of patients. Punch biopsies are also not helpful in diagnosing adenoma malignum. Instead, a deep wedge or cone biopsy is necessary to demonstrate the depth of glandular penetration. Frequently, adenoma malignum is misdiagnosed as a benign condition, and the accurate diagnosis only becomes apparent after the patient has undergone an extra fascial hysterectomy.
Treatment
The recommended treatment for local adenoma malignum (minimum deviation adenocarcinoma) in operable cases includes surgical intervention. The prognosis for such cases appears very good when the disease is operable. Additionally, adjuvant (chemo)radiation may be administered postoperatively for cases with high-risk features. Although several of these tumors are radioresistant, I typically avoid radiating these tumors. It's important to note that for more advanced cases of adenoma malignum, lymph node metastases are common, and the overall prognosis is poorer.
Based on the Korean paper (see below), risk factors include
| Risk Factor |
|---|
| Vaginal Invasion (VI) |
| Parametrial Invasion (PMI) |
| Resection Margin (RM) |
| Nodal Status |
| Lymphovascular Invasion (LVI) |
Patients without identified risk factors exhibited a recurrence-free survival (RFS) of 97.0% at three years. In contrast, those with more than one of the risk factors had a 3-year RFS of 65.4%
Two recent papers to read:


In my personal experience, Bevacizumab works in stabilizing the growth of these tumors. The MSKCC paper seems to suggest that ERBB2 mutations in these tumors might make them suseptible to trastuzumab.
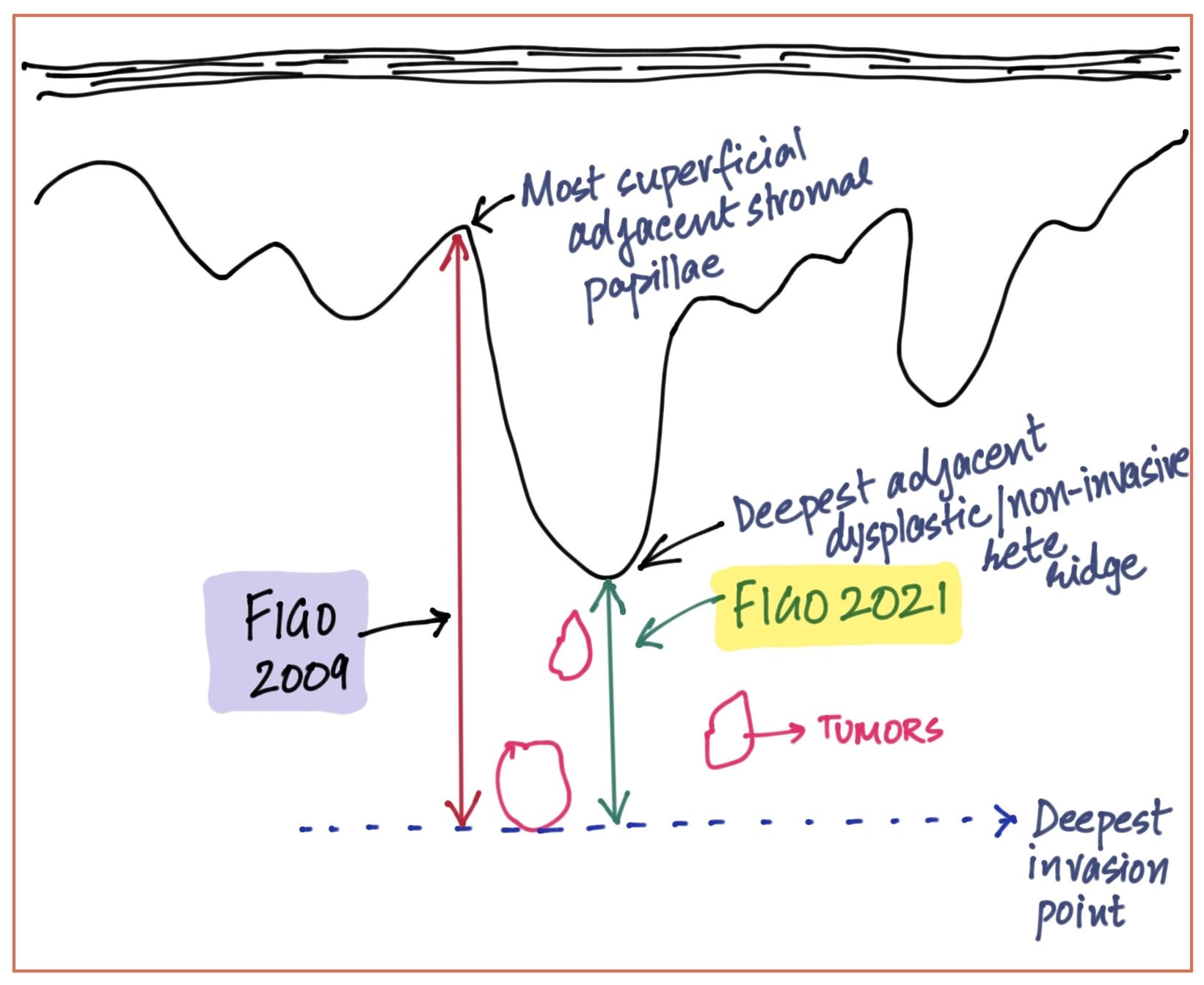
Vulvar Cancer (Publications Update # 46)
The debate on measuring the depth of invasion in vulvar cancer has intensified since the 2021 FIGO guidelines changed the standard measurement guidelines.
YOU MIGHT BE ASKED TO DRAW THIS !!
Neuroendocrine tumors of the Cervix (Publications Update # 48)
Diagnosis
PET-CT is significantly better than contrast CT, leading to changes in diagnosis and treatment for nearly one-third of patients based on PET scan results.

Order a PET scan for diagnostic workup of neuroendocrine tumors of the cervix

